my hands and foots are cold most of the time. what could be the cause and how to prevent.
Based on your description, your home sleep test raises some potential concerns, despite a normal Apnea-Hypopnea Index (AHI). Here are some considerations and insights tailored to your situation: 1. Oxygen Desaturation Concerns: An oxygen saturation level dropping to 78% is significant. Normally, oxyRead more
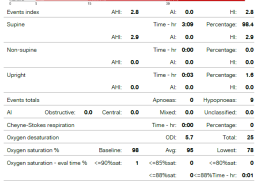
Based on your description, your home sleep test raises some potential concerns, despite a normal Apnea-Hypopnea Index (AHI). Here are some considerations and insights tailored to your situation:
1. Oxygen Desaturation Concerns: An oxygen saturation level dropping to 78% is significant. Normally, oxygen saturation during sleep should remain above 90%. A desaturation to 78% can suggest episodes of hypoxemia. This finding warrants further investigation, as recurrent or severe hypoxemia can have adverse effects, including those on cardiovascular and neurocognitive health.
2. Hypopnea Episodes: The presence of hypopneas, even with a normal AHI, is noteworthy. It’s important to consider which criteria were used to define hypopneas, as some definitions emphasize oxygen desaturation while others focus on EEG arousals. Both can contribute to reduced sleep quality and daytime symptoms like fatigue and sleepiness.
3. Limitations of Home Sleep Tests: While home sleep tests can be convenient, they often have limitations in detecting certain types of sleep-disordered breathing, particularly those without significant apneas or if events occur primarily in REM sleep or specific positions not well captured at home. Home tests also typically have limited channels compared to a full in-lab polysomnography (PSG), which can provide more comprehensive data.
4. Respiratory Effort-Related Arousals (RERAs): Consider whether the term RDI (Respiratory Disturbance Index), which includes RERAs, was evaluated. If there were RERAs present, they might explain the discrepancy between your symptoms and a normal AHI.
5. Clinical Correlation: It’s important to correlate these findings with your clinical symptoms and history. Persistent symptoms, such as the choking sensation your wife observed and any associated daytime sleepiness or fatigue, should be evaluated further.
Recommendations:
– Follow-Up with a Sleep Specialist: Discuss these findings with a sleep specialist. They might recommend an in-lab polysomnography for a more thorough evaluation, which could include measuring additional parameters like sleep stages and more nuanced respiratory effort assessment.
– Lifestyle and Environmental Modifications: Until further evaluation, consider lifestyle modifications such as weight management, positional therapy (avoiding supine sleep which can exacerbate obstructive events), and avoiding alcohol or sedatives before bed, as these can worsen sleep-disordered breathing.
– Additional Monitoring: In some cases, repeated or more detailed monitoring might be suggested, especially if initial investigations do not clearly explain your symptoms.
Given the complexity and the potential for significant health implications, a detailed clinical assessment is critical to effectively interpret your sleep study results and guide appropriate treatment.
Remember, individualized evaluation and management based on a comprehensive review of both clinical data and personal symptoms are key in sleep medicine.
See less
Experiencing cold hands and feet frequently can be attributed to a variety of factors, ranging from benign physiological responses to more serious underlying medical conditions. Here are some potential causes and preventive measures to consider: Potential Causes 1. Physiological Responses: - VasoconRead more
Experiencing cold hands and feet frequently can be attributed to a variety of factors, ranging from benign physiological responses to more serious underlying medical conditions. Here are some potential causes and preventive measures to consider:
Potential Causes
1. Physiological Responses:
– Vasoconstriction: In response to cold temperatures, blood vessels constrict to preserve core body heat, which can lead to cold extremities.
– Raynaud’s Phenomenon: This condition causes intermittent vasospasm of the small blood vessels in the fingers and toes, leading to episodes of color change (white, blue, red) and coldness, often triggered by cold or stress.
2. Circulatory Issues:
– Peripheral Artery Disease (PAD): Reduced blood flow due to narrowed arteries can result in coldness in the extremities, often accompanied by pain or cramping during physical activity.
– Diabetes: Poor circulation and neuropathy associated with diabetes can lead to cold extremities.
3. Neurological Conditions:
– Peripheral Neuropathy: Damage to peripheral nerves can disrupt normal temperature sensation, leading to feelings of coldness in the hands and feet.
4. Hormonal Factors:
– Hypothyroidism: An underactive thyroid can slow metabolism and reduce heat production, resulting in cold extremities.
– Anemia: Low hemoglobin levels can impair oxygen delivery to tissues, leading to coldness.
5. Lifestyle Factors:
– Smoking: Nicotine causes vasoconstriction, reducing blood flow to the extremities.
– Sedentary Lifestyle: Lack of physical activity can impair circulation.
Preventive Measures
1. Dress Appropriately:
– Wear warm, layered clothing, including thermal socks and gloves, to maintain body heat. Mittens are often warmer than gloves due to reduced surface area exposure.
2. Improve Circulation:
– Engage in regular physical activity to promote blood flow. Activities such as walking, cycling, or swimming can enhance circulation.
3. Manage Stress:
– Stress management techniques, such as yoga, meditation, or deep-breathing exercises, can help reduce episodes of Raynaud’s phenomenon.
4. Avoid Smoking:
– Quitting smoking can improve circulation and reduce vasoconstriction.
5. Diet and Hydration:
– Maintain a balanced diet rich in iron and vitamins to support overall health. Staying hydrated can also help maintain good circulation.
6. Warm Environment:
– Keep your living and working spaces warm, especially during colder months. Consider using heating pads or warm water soaks for your hands and feet.
7. Medical Consultation:
– If symptoms persist or are accompanied by pain, color changes, or ulcers, it is crucial to consult a healthcare professional. They may perform diagnostic tests to rule out conditions such as PAD, diabetes, or thyroid dysfunction.
Conclusion
Cold hands and feet can be a common issue, but understanding the underlying causes is essential for effective management. By implementing preventive measures and seeking medical advice when necessary, you can improve your symptoms and overall quality of life. If you have any specific concerns or if your symptoms worsen, please consult a healthcare provider for a thorough evaluation and tailored management plan.
See less