I have been working night shifts for a few months now. i cant really sleep more than 5 hours during the day and dont feel rested after that also. my friend asked me to try melatonin but I heard got ...
The ketogenic (keto) diet, characterized by high-fat, moderate-protein, and very low-carbohydrate intake, has gained popularity for various health conditions, including polycystic ovary syndrome (PCOS). However, its suitability for someone with PCOS requires careful consideration of several factors:Read more
The ketogenic (keto) diet, characterized by high-fat, moderate-protein, and very low-carbohydrate intake, has gained popularity for various health conditions, including polycystic ovary syndrome (PCOS). However, its suitability for someone with PCOS requires careful consideration of several factors:
Benefits of the Keto Diet for PCOS:
1. Insulin Sensitivity: PCOS is often associated with insulin resistance. The keto diet can potentially improve insulin sensitivity by significantly reducing carbohydrate intake, which in turn lowers insulin levels and helps stabilize blood glucose.
2. Weight Loss: Many women with PCOS struggle with weight management due to metabolic disturbances. The keto diet can be effective for weight loss, which may improve PCOS symptoms such as menstrual irregularities and ovulatory function.
3. Decrease in Androgen Levels: By improving insulin sensitivity and promoting weight loss, the keto diet might help lower androgen levels. This can be beneficial for reducing symptoms like hirsutism and acne.
Considerations and Potential Risks:
1. Nutritional Balance: The very restrictive nature of the keto diet might lead to deficiencies in essential nutrients if not carefully managed. It’s important to ensure that even while on a keto diet, individuals consume a variety of nutrients to maintain overall health.
2. Sustainability: The keto diet’s strict regimen can be difficult to maintain long term. Often, lifestyle changes that are sustainable and balanced are recommended for long-term health benefits and symptom management.
3. Lipid Profile Changes: The high fat content of the keto diet can alter lipid profiles, potentially increasing cardiovascular risk factors. Regular monitoring of lipid levels is advisable, especially for women with PCOS who may already have an elevated risk of cardiovascular issues.
4. Gut Health: Reduced fiber intake due to limited carbohydrates can affect gut health and lead to gastrointestinal issues.
Recommendations for Healthcare Professionals:
– Personalized Approach: Evaluate the individual’s specific health status, metabolic profile, and personal preferences before recommending a keto diet.
– Monitoring and Support: If a patient with PCOS chooses to pursue a keto diet, consider regular follow-up to monitor metabolic parameters, dietary balance, and overall health.
– Alternative Nutritional Plans: Consider other dietary interventions like the Mediterranean diet, which may offer a balanced approach with proven benefits for metabolic health and is easier to maintain.
– Multidisciplinary Collaboration: Engage with dietitians and nutritionists to help design a keto diet plan that is balanced and meets nutritional requirements while considering the individual’s lifestyle and health goals.
Conclusion:
While the keto diet may benefit some women with PCOS, it should be approached cautiously and on an individual basis, considering both the potential benefits and the challenges. Tailored nutritional counseling and continuous monitoring remain critical to ensure both efficacy and safety.
See less


Transitioning to night shift work can indeed be challenging due to the desynchronization between your internal circadian rhythms and your sleep-wake cycle. This can lead to insufficient sleep and compromised daytime functioning, which you seem to be experiencing. Here are some considerations and strRead more
Transitioning to night shift work can indeed be challenging due to the desynchronization between your internal circadian rhythms and your sleep-wake cycle. This can lead to insufficient sleep and compromised daytime functioning, which you seem to be experiencing.
Here are some considerations and strategies you can adopt:
1. Sleep Environment:
– Optimize your sleep environment: Ensure your bedroom is as dark as possible. Use blackout curtains or an eye mask and make sure the room is quiet and cool to simulate night-time conditions.
– Consider white noise or earplugs to block out daytime disturbances.
2. Sleep Hygiene Practices:
– Stick to a consistent sleep schedule, even on days off, to stabilize your body’s circadian rhythm.
– Develop a relaxing pre-sleep routine, such as reading or taking a bath, to help signal your body it’s time for sleep.
3. Exposure to Light:
– Before your shift: Bright light exposure at the start of your night shift can help stimulate alertness.
– After your shift: Wear sunglasses on your way home to reduce bright light exposure and signal to your body that it’s time to wind down.
4. Melatonin Supplementation:
– Melatonin Use: Melatonin can help adjust your sleep cycle, particularly if taken one to two hours before your desired sleep time in doses ranging from 0.5 to 3 mg. It may be beneficial for short-term regulation until your body adjusts, but use it strategically if your shift work schedule is inconsistent.
– Potential Side Effects: While melatonin is generally considered safe, you might experience daytime drowsiness, dizziness, or mild gastrointestinal symptoms. Considering these side effects, melatonin is generally favored over prescription sleeping pills, given its lower risk of dependency and fewer cognitive impairments.
5. Nutrition and Stimulants:
– Limit caffeine and heavy meals close to bedtime, as they can disrupt sleep.
– Stay well-hydrated but avoid large drinks before sleep to minimize disturbances.
6. Exercise:
– Regular physical activity can enhance sleep quality, but try to avoid vigorous exercise close to your sleep time.
7. Considerations on Sleep Aids:
– Prescription sleep medications, or sleeping pills, have more significant side effects and potential for dependency. They’re generally not recommended as a first-line option for shift work disorder unless other strategies fail.
8. Consultation:
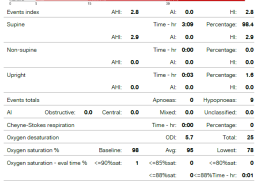
– If your difficulties persist, it may be beneficial to consult with a healthcare professional. They can rule out other sleep disorders like insomnia or sleep apnea, which might be contributing to your poor sleep.
Long-term Adjustment:
See lessAdapting to night shift work takes time, and your strategies may need adjustment based on how your body responds. Keep monitoring your progress and be open to refining your approach to optimize your sleep and daily function.